Snoring and Breathing Quality: Insights from a Wesper User Population

Introduction
Sleep Apnea (SA) is a group of breathing-related sleep disorders that result in inconsistent breathing and reduced airflow during sleep. SA is the second most common sleep disorder, with 26% of men and 10% of women in the United States affected. Snoring is one of the most common symptoms of OSA, with the incidence of snoring in SA patients ranging from 20% to 70% [1]. Studies have also shown a correlation between snoring intensity (decibel level) with SA severity [2]. This study aimed to evaluate the Wesper user population to determine if there is a relationship between the presence of snoring and snoring duration, with reduced breathing quality. We also investigated how sex influences snoring and breathing quality.
Methods
Our study population included all Wesper users that successfully tested with the Wesper 3-component system (n = 164), which consists of 2 Wesper patches applied to the abdomen and thorax and a finger pulse oximeter. Users were divided into two groups – users with captured snoring data and users without captured snoring data. Users were further filtered by sex to determine if sex impacts snoring and breathing quality. Two users who did not identify as male or female were excluded from the gender analysis. Metrics used for this analysis include the positive or negative presence of snoring on at least one Wesper test, mean snoring duration (minutes) across all Wesper tests completed, mean Apnea/Hypopnea Index (AHI), across all Wesper tests completed, and sex.
This study aimed to answer the following questions:
- The distribution of snoring users (users that have any tests with snoring recorded) vs. non-snoring users (users with snoring capture enabled but no identified snoring).
- The distribution of sex (male and female) in snoring vs. non-snoring users.
- The average AHI in snoring vs. non-snoring users.
- The average AHI in male snorers vs. male non-snorers.
- The average AHI in female snorers vs. female non-snorers.
- The average snoring duration vs. the average AHI severity in all snoring users.
- The average snoring duration vs. the average AHI severity in all snoring male users.
- The average snoring duration vs. the average AHI severity in all snoring female users.
- The average percentage of tests that are positive for snoring for snoring users.
- The average percentage of test that are positive for snoring for female snoring users.
-
The average percentage of tests that are positive for snoring for male snoring users.
12. The average percentage of tests that are positive for snoring vs. AHI severity level. - The average percentage of tests that are positive for snoring vs. AHI severity level in females.
- The average percentage of tests that are positive for snoring vs. AHI severity level in males.
Findings
Population Demographics
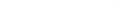
The tested population was made up of 49% non-snoring users (N = 81) and 51% snoring users (N=83; Figure 1). Of the snoring population, 29% were women and 71% were men, respectively (Figure 2). Of the non-snoring population, 27% were women and 73% were men, respectively (Figure 3). The Wesper female user population was made up of 52% snoring-women and 48% non-snoring women (Figure 4). Likewise, the Wesper male user population was made up of 49% snoring-men and 51% non-snoring men (Figure 5), demonstrating equal demographic distribution across snoring and non-snoring users.

Figure 1: Percentage of snorers vs. non-snorers in the Wesper user population.

Figure 2: Percentage of snoring women vs. snoring men in the Wesper user population.
Figure 3: Percentage of non-snoring women vs. non-snoring men in the Wesper user population.

Figure 4: Percentage of snoring women vs. non-snoring women in the Wesper user population.

Figure 5: Percentage of snoring men vs. non-snoring men in the Wesper user population.
Snoring vs. AHI
We first aimed to understand if there is a relationship between the presence of snoring and the duration of snoring with breathing quality. First, we measured the percentage of snoring-users with an elevated AHI vs. a normal AHI. Of the snoring-users, 70% had at least a mildly elevated AHI (AHI = 5-14; Figure 6), whereas only 41% of non-snoring users were found to have an elevated AHI (Figure7). This demonstrates that snoring is more likely to be associated with poor breathing quality, across all users.

Figure 6: Percentage of snoring users with an elevated AHI in the Wesper population

Figure 7: Percentage of non-snoring users with an elevated AHI in the Wesper population.

Figure 8: The average AHI in snoring users vs. non-snoring users, regardless of gender
In snoring-users, a longer average snoring duration (minutes) was found to be positively related to a higher average AHI severity level (Table 1; Figure 9), regardless of gender.
Table 1: User AHI severity vs. average snoring duration
|
AHI Severity |
Average Snoring Duration (Min) |
|
Severe (AHI >30) |
70 |
|
Moderate (AHI 15-30) |
68 |
|
Mild (AHI 5-14) |
58 |
|
Normal (AHI <5) |
42 |

Figure 9: User AHI severity vs. average snoring duration, regardless of gender
Specifically, is there a relationship between habitual (chronic) snoring with AHI severity, i.e. do individuals who snore nightly have a higher average AHI than individuals who snore occasionally?
In the snoring population, 93% of users with snoring data captured had positive snoring on at least half (50%) of their tests. 78% of users with snoring data captured has positive snoring on at least 3 quarters (75%) of their tests. 46% of users with snoring data captured had positive snoring on all (100%) of their tests (Figure 10).

Figure 10: Percentage snoring-positive users with snoring on 50%, 75%, and 100% of Wesper tests.
Next, we evaluated how snoring consistency in the snoring population affected AHI severity. 100% of users with an average severe AHI were positive for snoring on at least 50% of their tests. Similar trends were seen in moderate (92%), mild (92%), and normal users (94%). Demonstrating that all snoring users, regardless of AHI, had snoring for at least half of all tests taken (Figure 11).

Figure 11: Percentage of snoring-positive users with snoring recorded on at least 50% of their Wesper tests.
Increasing the threshold 75% (Figure 12), 85% (Figure 13), and 100% (Figure 14) demonstrated that a severe AHI has a positive relationship with chronic, habitual (nightly) snoring, however the relationship is lower in individuals with normal – moderate AHI.

Figure 12: Percentage of snoring-positive users with snoring recorded on at least 75% of their Wesper tests.
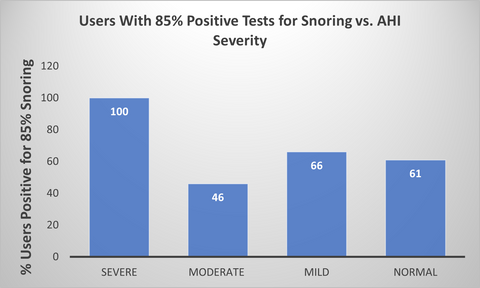
Figure 13: Percentage of snoring-positive users with snoring recorded on at least 85% of their Wesper tests.

Figure 14: Percentage of snoring-positive users with snoring recorded on at least 100% of their Wesper tests.
Sex Differences in Snoring vs. Non-Snoring Users
We evaluated if snoring affects breathing quality differently in women and men. First, we measured the percentage of female snoring-users with an elevated AHI vs. a normal AHI. Of the female snoring-users, 61% had at least a mildly elevated AHI (AHI = 5-14; Figure 15), whereas only 38% of non-snoring users were found to have an elevated AHI (Figure 16). This demonstrates that snoring is more likely to be associated with poor breathing quality in women.

Figure 15: Percentage of snoring women with an elevated AHI in the Wesper population.

Figure 16: Percentage of non-snoring women with an elevated AHI in the Wesper population.
Of the male snoring-users, 72% had at least a mildly elevated AHI (AHI = 5-14; Figure 17), whereas only 41% of non-snoring users were found to have an elevated AHI (Figure 18). This demonstrates that snoring is more likely to be associated with poor breathing quality in men.

Figure 17: Percentage of snoring men with an elevated AHI in the Wesper population.

Figure 18: Percentage of non-snoring men with an elevated AHI in the Wesper population.
Next, we examined average AHI in female and male snorers and non-snorers. Data analysis showed that snoring users had a higher average AHI than non-snoring users, regardless of sex (Figure 19), demonstrating that the positive relationship between snoring and AHI is maintained in both men and women. Snoring men, however, showed a larger increase in AHI compared to men who didn’t snore (51% increase), than snoring women compared to women who didn’t snore (24% increase). This is despite a similar average AHI in non-snoring men (AHI = 6.22) and non-snoring women (AHI = 7.04).
Snoring duration was longer on average in users with a higher average AHI severity for women (Figure 20) and men (Figure 21), demonstrating that snoring duration is positively associated with breathing severity in men and women. However, it’s important to note that there were no female users with snoring that fell into the severe (AHI = >30) category.

Figure 19: Average AHI in snoring-men vs. non-snoring men and snoring women vs. non-snoring women.

Figure 20: Average AHI severity vs. average snoring duration in snoring-women.

Figure 21: Average AHI severity vs. average snoring duration in snoring-men.
Finally, we aimed to understand if habitual (chronic) snoring affects women and men differently. Only users with at least 3 completed tests were considered for this analysis (N = 20 Women; N = 37 Men). Snoring consistency was broken down into percentages of user tests with snoring data captured.In the snoring female population, 95% of women with snoring data captured had positive snoring on at least half (50%) of their Wesper tests. 75% of snoring women had positive snoring on at least ¾ (75%) of their Wesper tests. 55% of snoring women had positive snoring on all (100%) of their tests (Figure 22)

Figure 22: Percentage snoring-positive users with snoring on 50%, 75%, and 100% of Wesper tests.
Next, we evaluated how snoring consistency in the female snoring population affected AHI severity. It is important to note that there were no female snorers with a severe AHI recorded. 80% of users with a moderate AHI were positive for snoring on at least 50% of their tests. 100% of mild and normal users had positive snoring on at least 50% of their Wesper tests. This demonstrated that nearly all snoring users, snored on at least 50% of their tests, regardless of their AHI severity.

Figure 23: Percentage of snoring-positive female users in the moderate, mild, and normal AHI severity range, with snoring recorded on at least 50% of their Wesper tests
When the snoring-positive threshold was raised to 75% of tests, 60% of users with a moderate AHI were positive for snoring. 100% of mild users were positive for snoring and 71% of normal users were positive for snoring (Figure 24).

Figure 24: Percentage of snoring-positive female users in the moderate, mild, and normal AHI severity range, with snoring recorded on at least 75% of their Wesper tests.
When the snoring-positive threshold was raised to 85% of tests, 40% of users with a moderate AHI were positive for snoring. 62% of mild users were positive for snoring and 71% of normal users were positive for snoring (Figure 25).

Figure 25: Percentage of snoring-positive female users in the moderate, mild, and normal AHI severity range, with snoring recorded on at least 85% of their Wesper tests.
When the snoring-positive threshold was raised to 100% of tests, 40% of users with a moderate AHI were positive for snoring. 50% of mild users were positive for snoring and 71% of normal users were positive for snoring (Figure 26). This data demonstrates that there is no clear relationship between frequency of snoring on Wesper tests and AHI severity in women.

Figure 26: Percentage of snoring-positive female users in the moderate, mild, and normal AHI severity range, with snoring recorded on at least 100% of their Wesper tests.
In the snoring male population, 86% of men with snoring data captured had positive snoring on at least half (50%) of their Wesper tests. 76% of snoring men had positive snoring on at least ¾ (75%) of their Wesper tests. 39% of snoring women had positive snoring on all (100%) of their tests (Figure 27)

Figure 27: Percentage male snoring-positive users with snoring on 50%, 75%, and 100% of Wesper tests.
Next, we evaluated how snoring consistency in the male snoring population affected AHI severity. 100% of users with a severe and moderate AHI were positive for snoring on at least 50% of their tests. 89% of users with a mild AHI were positive for snoring on at least 50% of their tests. 83% of normal users had positive snoring on at least 50% of their Wesper tests. This demonstrated that nearly all snoring users, snored on at least 50% of their tests, regardless of their AHI severity.

Figure 28: Percentage of snoring-positive female users in the moderate, mild, and normal AHI severity range, with snoring recorded on at least 100% of their Wesper tests.
When the snoring-positive threshold was raised to 75% of tests, 100% of users with a severe and moderate AHI were positive for snoring. 67% of mild users were positive for snoring and 75% of normal users were positive for snoring (Figure 29).
Figure 29: Percentage of snoring-positive male users in the moderate, mild, and normal AHI severity range, with snoring recorded on at least 75% of their Wesper tests.
When the snoring-positive threshold was raised to 85% of tests, 100% of users with a severe AHI were positive for snoring. 50% of moderate users were positive for snoring, 55% of mild users were positive for snoring, and 71% of normal users were positive for snoring (Figure 30).

Figure 30: Percentage of snoring-positive male users in the moderate, mild, and normal AHI severity range, with snoring recorded on at least 85% of their Wesper tests.
When the snoring-positive threshold was raised to 100% of tests, 100% of users with a severe AHI were positive for snoring. 50% of moderate users were positive for snoring, 27% of mild users were positive for snoring, and 41% of normal users were positive for snoring (Figure 31). This demonstrates that in men, a severe AHI is associated with habitual chronic snoring.

Figure 31: Percentage of snoring-positive male users in the moderate, mild, and normal AHI severity range, with snoring recorded on at least 100% of their Wesper tests.
Discussion
Clinical studies have shown that anywhere from 20-70% of people with OSA snore, and snoring intensity (measured in decibels) is positively correlated with AHI. This analysis aimed to identify if snoring is associated with worse breathing quality in the Wesper user population, and if sex plays a role in this relationship.
This analysis demonstrated that in the Wesper user population, approximately half of users that enabled snoring capture on their Wesper device had some level of snoring on their tests. Snoring percentages were evenly distributed between men and women users, despite the majority of users tested being male.
There was a positive relationship between the presence of snoring and AHI in both men and women. We also identified that snoring duration was associated with higher AHI severity, in which the longer an individual snores on average, the higher their average AHI severity was likely to be.
When evaluation whether the consistency of snoring on Wesper tests was associated with AHI severity, there was only a positive association in men with a severe AHI. There was no positive association in women, however there were no female-snorers in the severe AHI range captured.
Interestingly, despite both male and female users demonstrating similar trends, snoring appeared to have an overall stronger association with poor breathing quality in men than women. This aligns with the “gender bias” hypothesis that women with SDB are less likely to present with traditional OSA symptoms [3], leading to providers disregarding their risk.
Studies have also found that women tend to have less severe OSA than males, with a lower AHI and shorter apneas and hypopneas [4]. This leads to lower testing and diagnosis rates in females with SDB than men, despite the consequences of the disease being the same in both sexes.
Conclusion
Wesper user data showed a positive association between the presence of snoring and snoring duration with poor breathing quality in both males and females. A small association with habitual (chronic) snoring in men with severe poor breathing quality was also identified. Thus, any level of snoring should prompt screening for SDB. This study also concluded that while snoring in women is a common symptom of SDB, women with SDB are less likely to snore than men. OSA in women should, therefore, not be ruled out by health professionals if snoring isn’t present.
References
- Keropian B, Murphy N. The prevalence of OSA in snorers presenting with various chief complaints: a pilot study. Cranio. 2014 Jul;32(3):217-8. doi: 10.1179/0886963414Z.00000000032. Epub 2014 Apr 14. PMID: 25000164.
- Maimon N, Hanly PJ. Does snoring intensity correlate with the severity of obstructive sleep apnea? J Clin Sleep Med. 2010 Oct 15;6(5):475-8. PMID: 20957849; PMCID: PMC2952752.
- Young T, Hutton R, Finn L, Badr S, Palta M. The gender bias in sleep apnea diagnosis. Are women missed because they have different symptoms? Arch Intern Med. 1996 Nov 25;156(21):2445-51. PMID: 8944737.
- Wimms A, Woehrle H, Ketheeswaran S, Ramanan D, Armitstead J. Obstructive Sleep Apnea in Women: Specific Issues and Interventions. Biomed Res Int. 2016;2016:1764837. doi: 10.1155/2016/1764837. Epub 2016 Sep 6. PMID: 27699167; PMCID: PMC5028797.